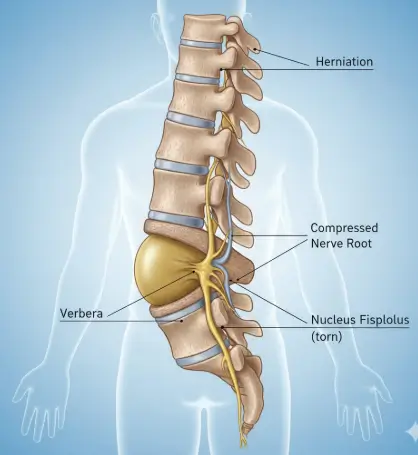
A herniated disc happens when the soft part inside a spinal disc pushes out through its outer layer. This can press on nearby nerves and cause pain, numbness, or weakness in your back, arms, or legs. Herniated discs are a common reason for back and neck problems. Knowing the signs early can help you get treatment faster and avoid making the problem worse.
Symptoms can be different for everyone. Some people feel sudden, sharp pain, while others notice pain that slowly gets worse over time. Learning the common symptoms, causes, and ways to check for a herniated disc can help you take care of your spine.
What Is a Herniated Disc and How Does It Happen?
A herniated disc happens when one of the discs in your spine gets damaged. Spinal discs are soft cushions between your vertebrae (the bones in your spine). They act like shock absorbers, helping you bend, twist, and move without pain.
When a disc herniates, the soft inner part pushes out through a tear in the outer layer. This can irritate or press on nearby nerves, which may cause pain, numbness, or weakness.
Herniated discs are more likely to happen because of:
- Age and wear: Discs can weaken as you get older.
- Injury or heavy lifting: Sudden twists, falls, or lifting heavy objects can cause a disc to herniate.
- Poor posture or repetitive stress: Slouching for long periods or doing repeated bending and twisting motions can increase the risk.
- Genetics: Some people are more likely to have weak discs.
Knowing how herniated discs happen can help you prevent injuries and notice problems early.
How to Know If You Have a Herniated Disc
Recognizing a herniated disc early can help you get the right treatment and prevent more serious problems. Doctors usually look at your symptoms, medical history, and physical exam results to make a diagnosis.
Signs to Watch For
- Persistent back or neck pain: Pain that does not improve with rest or over-the-counter medication.
- Pain that radiates: Pain spreading down your arms or legs, often described as sharp, burning, or shooting.
- Numbness or tingling: Pins-and-needles or tingling sensations in your arms, hands, legs, or feet.
- Muscle weakness: Weakness that affects walking, lifting, or gripping objects.
- Changes in reflexes: Reduced or slower reflexes in the knees, elbows, or other areas.
When to See a Doctor
- Pain that gets worse over time.
- Numbness, tingling, or weakness in the arms or legs.
- Difficulty controlling your bladder or bowels (seek emergency care).
Diagnosis Methods
Doctors may use:
- Physical exam: Checking your strength, reflexes, and range of motion.
- Imaging tests: X-rays, MRI, or CT scans can show which disc is affected.
- Nerve tests: Sometimes, tests like EMG can check how well your nerves are working.
Clinical Note: Not all back pain is caused by a herniated disc. Seeing a doctor ensures you get the right diagnosis and treatment plan.
Causes and Risk Factors of a Herniated Disc
A herniated disc happens when the soft inner part of a spinal disc pushes through its outer layer. Certain factors can make it more likely to happen.
Age and Wear
- Discs naturally lose water and flexibility as you get older.
- This makes them weaker and more likely to tear or bulge.
Injury or Trauma
- Sudden injuries, like falls or car accidents, can damage discs.
- Lifting heavy objects incorrectly or twisting your back suddenly can also cause a herniation.
Repetitive Stress
- Repeated bending, twisting, or lifting can put stress on your discs over time.
- Poor posture while sitting, standing, or using a computer can increase risk.
Genetics
- Some people are naturally more prone to weak or damaged discs.
Other Health Factors
- Smoking can reduce blood flow to discs and slow healing.
- Being overweight puts extra pressure on the spine, increasing the chance of disc problems.
- A sedentary lifestyle can weaken the muscles that support your spine.
Note: Having one or more risk factors does not guarantee a herniated disc, but it makes it more likely. Paying attention to posture, exercise, and healthy habits can lower your risk.
How to Diagnose a Herniated Disc
If a doctor suspects you have a herniated disc, they will use a combination of exams and tests to confirm it. Early diagnosis helps prevent the problem from getting worse and guides treatment.
Medical History
- Your doctor will ask about your symptoms, when they started, and what makes them better or worse.
- They may also ask about past injuries, medical conditions, and daily activities.
Physical Examination
- The doctor will check your posture, spine movement, and muscle strength.
- Reflexes, sensation, and coordination may be tested to see if nerves are affected.
- You may be asked to bend, twist, or lift your legs to check for pain or nerve irritation.
Imaging Tests
- X-rays: Show the bones in your spine and can rule out other problems.
- MRI (Magnetic Resonance Imaging): Provides detailed images of discs and nerves to locate a herniation.
- CT Scan: Sometimes used if MRI is not possible or to get extra detail.
Other Tests
- Electromyography (EMG): Measures the electrical activity in muscles and can show nerve damage.
- Nerve Conduction Study (NCS): Checks how well nerves send signals to muscles.
Note: Diagnosis is based on a combination of your symptoms, physical exam, and test results. Not all herniated discs cause symptoms, so imaging alone may not always mean treatment is needed.

Treatment Options for a Herniated Disc
Most herniated discs improve without surgery. Treatment focuses on reducing pain, improving movement, and preventing further damage.
Non-Surgical Treatments
- Rest and activity changes: Avoid heavy lifting or twisting, but keep gentle movement to prevent stiffness.
- Medications: Over-the-counter pain relievers or anti-inflammatory medicines can reduce pain and swelling.
- Physical therapy: Exercises help strengthen muscles around your spine, improve flexibility, and support healing.
- Heat or cold therapy: Applying ice or heat packs can help reduce pain and muscle tension.
- Lifestyle changes: Maintaining a healthy weight, practicing good posture, and staying active can help your spine recover.
Medical Procedures
- Epidural steroid injections: In some cases, injections can reduce inflammation and relieve pain.
Surgical Treatments
Surgery is usually considered only if non-surgical treatments don’t help or if symptoms are severe. Common options include:
- Discectomy: Removing the part of the disc pressing on nerves.
- Laminectomy: Removing part of the bone covering the spinal canal to relieve pressure.
- Spinal fusion (rarely): Joining vertebrae to stabilize the spine.
Clinical Note: Your doctor will recommend herniated disc surgery based on your symptoms, the location of the herniated disc, and your overall health. Early care often leads to faster recovery.
When to See a Neurosurgeon
A neurosurgeon specializes in problems with the spine and nervous system. If you think you have a herniated disc, a neurosurgeon can check your spine and nerves and recommend the best treatment.
See a neurosurgeon if you have:
- Severe or worsening pain: Pain that does not get better with rest, medication, or physical therapy.
- Numbness or tingling: Pins-and-needles or loss of feeling in your arms, hands, legs, or feet.
- Muscle weakness: Weakness that makes it hard to lift, grip, or walk normally.
- Loss of bladder or bowel control: This is an emergency and requires immediate care from a neurosurgeon.
Other reasons to consult a neurosurgeon:
- Pain that spreads down your arms or legs and interferes with daily activities.
- Pain that persists despite conservative treatments like rest, exercise, or medications.
- Any concern about nerve damage or spinal instability.
Clinical Note: Early evaluation by a neurosurgeon can prevent permanent nerve damage and ensure you get the right treatment; whether it’s physical therapy, medications, injections, or surgery.
Frequently Asked Questions (FAQ)
1. Can a herniated disc heal on its own?
Yes. Many herniated discs improve over time with rest, physical therapy, and medication. However, severe cases may need a neurosurgeon’s evaluation.
2. How do I know if my nerves are affected?
Signs of nerve involvement include numbness, tingling, muscle weakness, or pain that radiates down your arms or legs. A neurosurgeon can run tests to check nerve function.
3. When is surgery necessary?
Surgery is usually considered if:
- Pain or weakness does not improve with non-surgical treatments.
- You have loss of bladder or bowel control.
- There is significant nerve compression causing worsening weakness or numbness.
4. Can I continue daily activities with a herniated disc?
Gentle movement and low-impact activities are usually safe. Avoid heavy lifting, twisting, or high-impact sports until cleared by a neurosurgeon.
5. Will a herniated disc cause permanent damage?
Most patients recover without long-term problems. Permanent nerve damage is rare but can happen if severe symptoms are ignored. Early evaluation by a neurosurgeon lowers this risk.
6. How can I prevent another herniated disc?
- Maintain good posture.
- Exercise regularly to strengthen your core.
- Lift objects safely, bend your knees, and avoid twisting.
- Maintain a healthy weight and avoid smoking.
7. Can a herniated disc come back after surgery?
It’s possible, especially if the spine experiences stress or poor posture after recovery. Neurosurgeons often give guidance on exercises and lifestyle changes to reduce the risk.